As the world recovers from the impact of the COVID-19 pandemic, leading experts and global health organizations are raising urgent warnings about the spread of rare and potentially deadly viruses into new regions in 2025. Several novel outbreaks—most notably of avian influenza H5N1, Marburg virus, Nipah virus, Mpox clade 1b, and Chikungunya—have expanded beyond their usual confines, prompting renewed fears of another global epidemic.
Rare Viruses Pushing New Boundaries
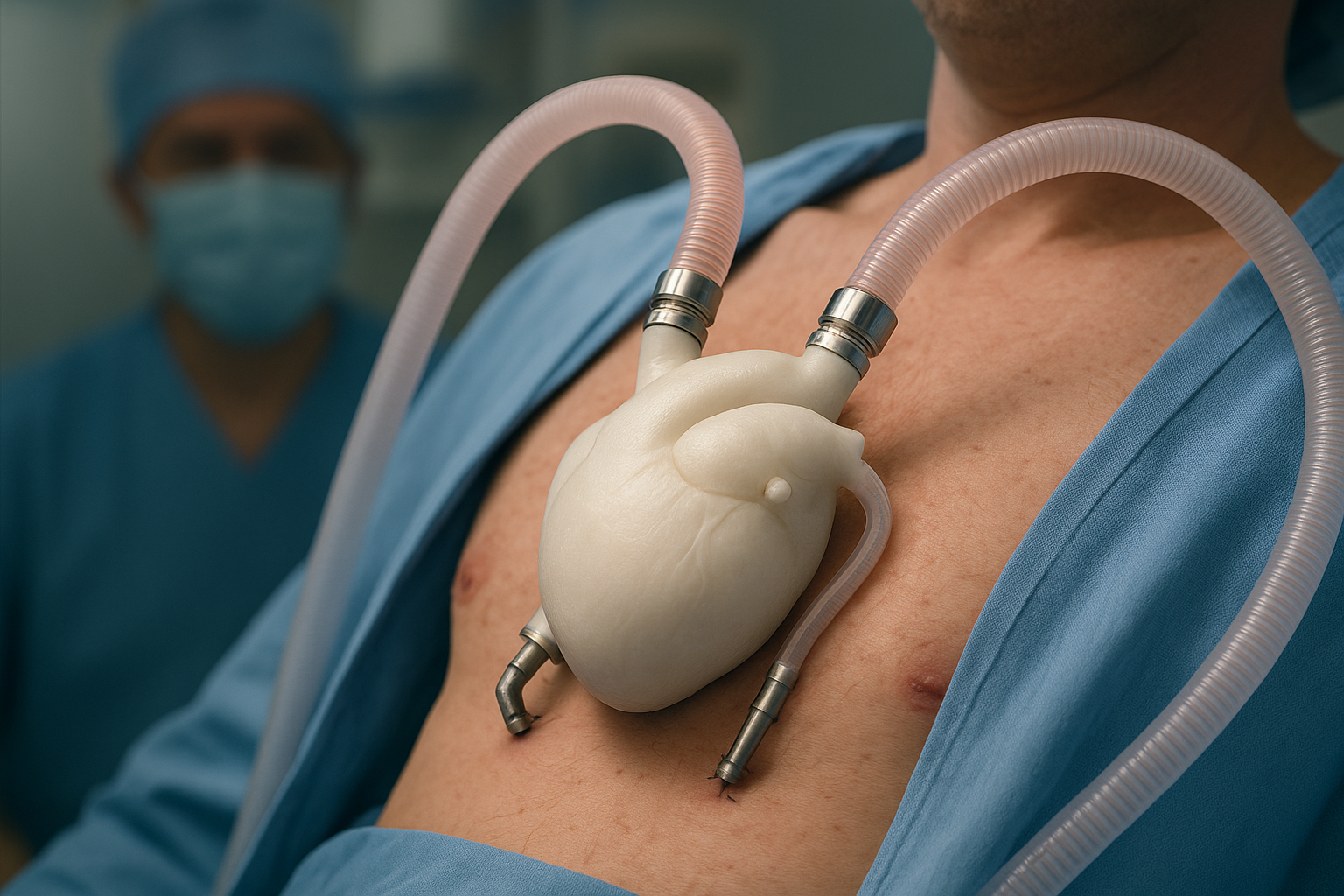
Highly Pathogenic Avian Influenza (H5N1)
-
Rapid Expansion: The H5N1 bird flu has moved from wildlife into domestic poultry and, in a concerning new trend, into dairy cattle across the United States. Over 1,000 cattle herds have been infected, with spillover to humans resulting in more than 70 confirmed cases and at least one death.
-
Mutation Risks: Experts fear that the increasing ability of H5N1 to infect mammals raises the possibility of the virus acquiring mutations that allow efficient human-to-human transmission, a crucial step toward pandemic potential.
-
Current Human Risk: Although the CDC maintains the public risk is currently low, health authorities are particularly concerned about those in close contact with infected animals. Pandemic preparedness strategies are being reviewed and stockpiles of vaccines are in place in some countries.
Marburg Virus Emergencies
-
Recent Outbreaks: Marburg virus, a highly infectious hemorrhagic fever similar to Ebola, has seen renewed outbreaks in Africa, particularly in Equatorial Guinea, Tanzania, and Rwanda since 2024.
-
Fatalities and Spread: The fatality rate in recent clusters has been extremely high, in some cases reaching 100%, underscoring the gravity of unchecked outbreaks.
-
Geographical Moves: Concerns have risen due to the first cases reported in regions with no prior incidence, increasing the global risk profile of this rare pathogen.
Mpox (Clade 1b Variant)
-
New Variant: Initially identified in the Democratic Republic of Congo, the mutated clade 1b of Mpox has demonstrated increased human-to-human transmissibility.
-
Global Expansion: After rapid spread in Central and East Africa, imported cases have appeared in Asia, Europe, and North America, attributed to increased international travel. Multiple isolated cases have been confirmed in the United States, Sweden, Thailand, and India, sparking wider surveillance and health checks at borders.
-
Control Measures: Authorities are urging enhanced disease surveillance, robust contact tracing, and cross-border cooperation to curb further transmission.
Nipah Virus
-
Recent Escalations: The Nipah virus, primarily transmitted by fruit bats but capable of human-to-human spread, has re-emerged in Southern India in 2025, causing alarm due to its high mortality and lack of approved treatments.
-
Outbreak Response: Intensive efforts are underway—including vaccine research and containment measures—to prevent broader dissemination of this deadly virus.
Chikungunya and Other Re-emerging Threats
-
Regional Surges: The World Health Organization has sounded an alarm on Chikungunya, with significant epidemics reported in Reunion, Mayotte, and Mauritius since early 2025.
-
Additional Risks: Measles, polio, and other infectious diseases are also resurging in new areas because of immunity gaps and shifting climate patterns, compounding global concerns.
Why 2025 Is Especially Alarming
Recent years have seen an uptick in the appearance and spread of rare and re-emerging diseases due to several interconnected factors:
-
Climate Change: Altered weather patterns are affecting the habitats and migration of disease-carrying animals.
-
Global Travel: High levels of international movement allow viruses to traverse continents swiftly.
-
Immunity Gaps: After the COVID-19 pandemic, waning herd immunity due to paused vaccination campaigns has created vulnerabilities to measles, polio, and other preventable diseases.
-
Viral Evolution: Increased interspecies transmission gives viruses more chances to mutate, potentially developing traits for easier human spread.
Expert Warnings and Calls to Action
Epidemiologists and virologists stress that the world remains dangerously underprepared for the next pandemic:
-
Dr. Sten H. Vermund (GVN, USF Health): Highlights the urgent need for proactive surveillance, robust animal and human health coordination, and rapid response if signs of adaptation for human-to-human spread emerge.
-
WHO and CDC Guidance: Emphasize ongoing vigilance, especially among those in high-risk occupational groups, and continued investment in pandemic preparedness infrastructure, diagnostics, and vaccine research.
What Governments and the Public Can Do
-
Surveillance: Implement robust early warning systems and expand genomic sequencing for rapid detection of emerging and mutating pathogens.
-
Border Health Measures: Enhance border controls, traveler screenings, and targeted quarantines as needed.
-
Vaccination: Address vaccination gaps among populations, and support research into new vaccines where none exist.
-
Public Communication: Ensure transparent, accurate public health communication to avoid panic but encourage vigilance and compliance with health directives.
The events of 2025 serve as a sharp reminder that rare viruses can—and do—emerge or re-emerge, crossing geographic boundaries and threatening global stability. While much has been learned since COVID-19, experts caution that complacency is not an option; the next pandemic may already be spreading, quietly, across new frontiers.